Controversy remains as to whether or not cell phones (hand held computers with audio capability) and iPads have a place in the operating room. It is true that they can be a distraction for healthcare workers but they also put a wealth of information at your finger tips. When used appropriately, they provide instant information to the anesthetist that could make a difference in patient safety.
Recently, I posed the question to several of my colleagues; What is your favorite Anesthesia APP? Below are a few of the favorites. I am asking porcrna.com readers the same question. What is your favorite APP? Look over the APPs listed below and use the comment box below to share your experience with these APPs or to add your own favorites.
 Epocrates: This free drug reference is the #1 mobile drug reference for U.S. physicians. With it you can search brand, generic, and OTC medicines. Plus, you can customize your homepage for quick access to the features you use most frequently.
Epocrates: This free drug reference is the #1 mobile drug reference for U.S. physicians. With it you can search brand, generic, and OTC medicines. Plus, you can customize your homepage for quick access to the features you use most frequently.
 abeoCoder gives access to CPT®, ASA CROSSWALKS®, and ICD codes right from your iPhone or BlackBerry. abeoCoder app provides you with codes, base units, descriptions and more.
abeoCoder gives access to CPT®, ASA CROSSWALKS®, and ICD codes right from your iPhone or BlackBerry. abeoCoder app provides you with codes, base units, descriptions and more.
Coding Made Easy.
 Pedi Safe is an advanced airway management and cardiac resuscitation app. In an emergency, healthcare providers can quickly identify a patient’s weight or Broselow color, and then Pedi Safe displays all appropriate weight based dosing, equipment sizes, and normal vital signs. An excellent reference for doctors, nurses and paramedics!
Pedi Safe is an advanced airway management and cardiac resuscitation app. In an emergency, healthcare providers can quickly identify a patient’s weight or Broselow color, and then Pedi Safe displays all appropriate weight based dosing, equipment sizes, and normal vital signs. An excellent reference for doctors, nurses and paramedics!
 drawMD; Using the iPad, Anesthesiologists can create interactive visual guides as a way to explain complex issues and possible medical and surgical solutions for Anesthesia and Critical Care-specific conditions and procedures, such as a central line chest tube, intubation, spinal epidural, etc.
drawMD; Using the iPad, Anesthesiologists can create interactive visual guides as a way to explain complex issues and possible medical and surgical solutions for Anesthesia and Critical Care-specific conditions and procedures, such as a central line chest tube, intubation, spinal epidural, etc.
One more just for fun…….and this one works on your pet too!
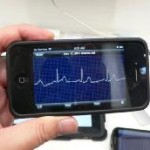
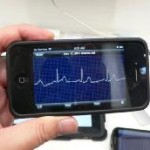 Alivecor has developed the iPhone ECG—a case that transforms the iPhone into a wireless, clinical quality heart monitor. The case is able to monitor one’s heart rate almost immediately, and can even measure through a cotton shirt!
Alivecor has developed the iPhone ECG—a case that transforms the iPhone into a wireless, clinical quality heart monitor. The case is able to monitor one’s heart rate almost immediately, and can even measure through a cotton shirt!
Browse, enjoy and leave a comment to share your favorite APP with your colleagues.