The evolving changes in the delivery of Healthcare in general and anesthsia in particular has created an emphasis on patient safety. With the push for more cost effective delivery of healthcare, more procedures are being done on an outpatient basis on sicker patients. Combining the new economics with the obesity epidemic in America has created the scenario where an increasing number of patients with Obstructive Sleep Apnea are presenting for outpatient surgery. As anesthetists, we are tasked with providing safe care and answering the question of who is or is not a candidate for outpatient surgery.
The evolving changes in the delivery of Healthcare in general and anesthsia in particular has created an emphasis on patient safety. With the push for more cost effective delivery of healthcare, more procedures are being done on an outpatient basis on sicker patients. Combining the new economics with the obesity epidemic in America has created the scenario where an increasing number of patients with Obstructive Sleep Apnea are presenting for outpatient surgery. As anesthetists, we are tasked with providing safe care and answering the question of who is or is not a candidate for outpatient surgery.
In 2006 the ASA published guidelines for the perioperative management of patients with OSA. Although the guidelines were good at the time, the Society for Ambulatory Anesthesia felt that the ASA guidelines were due for review and updating, did a comprehenhive review, and published their findings.
An article by Joshi et al published in Anesth Analg 2012 (Society for Ambulatory Anesthesia Consensus Statement on Preoperative Selection of Adult Patients with Obstructive Sleep Apnea Scheduled for Ambulatory Surgery) reviewed the ASA guidelines. They went on to note that the Society for Ambulatory Anesthesia task force on practice guidelines developed a consensus statement for the selection of patients with OSA scheduled for ambulatory surgery. Some key points include:
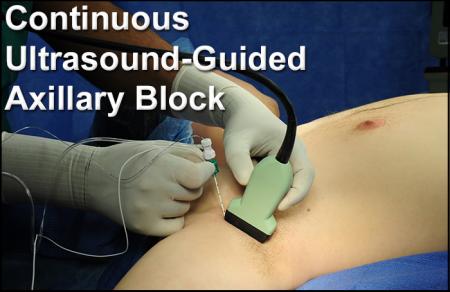
- Patients with a known diagnosis of OSA and optimized comorbid medical conditions can be considered for ambulatory surgery, if they are able to use a continuous positive airway pressure device in the postoperative period.
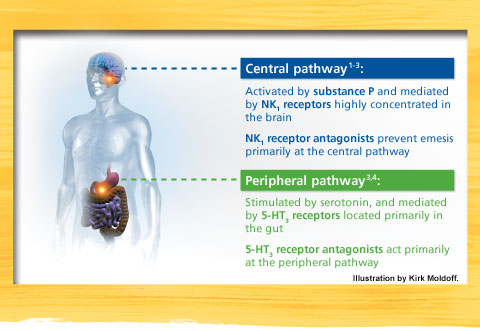
- Patients with a presumed diagnosis of OSA, based on screening tools such as the STOP–Bang questionnaire, and with optimized comorbid conditions, can be considered for ambulatory surgery, if postoperative pain can be managed predominantly with nonopioid analgesic techniques.
- On the other hand, OSA patients with nonoptimized comorbid medical conditions may not be good candidates for ambulatory surgery.
Click here for an abstract of the Joshi article.
As anesthetists, how do we assess patients and how do we determine who is at risk? The Society for Ambulatory Anesthesia recommends the use of the STOP-Bang assessment tool. The questionnaire asks 8 basic questions and gives the anesthtist valuable information about the OSA risk during the preoperative evaluation.
Click here for the STOP-Bang tool in a PDF format which can be downloaded and printed.
Combining a good physical evaluation with the STOP-Bang assessment will help identify those at risk and enable the anesthetist to make an informed decision regarding who should or should not receive outpatient care.