CRNAs are certified as qualified to practice by the Council on Certification and Recertification of Nurse Anesthetists. In addition, they must be licensed to practice nursing by the state in which they practice. Questions often arise regarding prescriptive authority and the legal ability to use controlled substances in our daily practice. Laws vary from state to state. Below is an excellent review of the Law of the State of Texas prepared by Pamela Chambers, CRNA. Contact Ms Chambers at Lex Terrae consulting if you have questions about the laws in your state.
 Submitted by Pamela Chambers, MSN, CRNA, EJD
Submitted by Pamela Chambers, MSN, CRNA, EJD
Every year new laws become effective that affect all of us. Some are so obscure that we never become aware of them – unless we violate them. As mentioned in earlier articles, ignorance of the law is rarely a defense to violating it. Two recent legislative changes (i.e. new laws) that affect nurse anesthesia practice are the new consent requirements and the controlled substance program requirements.
Title 25 of the Texas Administrative Code (Health Services) Part 7 (Texas Medical Disclosure Panel) Chapter 601 (Informed Consent) codifies the requirements of the Texas Civil Practice and Remedies Code, Chapter 74, Medical Liability, Subchapter C, section 74.102. In English: the new consent rules are laws that further explain the law regarding medical liability in Texas. The importance of this cannot be overstated. The new consent procedure, requiring a specific form to be completed and signed by the anesthesia practitioner, is a law. This is not “just another rule” designed to test our memory of rules. This new law was likely the result of changing health care realities (i.e. such as the patient who awakens from surgery having had procedures that were necessary but not specifically discussed prior to induction). When society changes we have the ability to change our laws to reflect the will of the electorate, and the good of society.
In an effort to protect society by controlling dissemination of federally controlled substances, the Texas Department of Public Safety (DPS) requires registration of all individuals who possess a DEA# for the purpose of prescribing, or dispensing controlled substances in the state of Texas. As with many of our laws in every state of the union, this instance derives from federal law.
In the State of Texas, relevant guidance pertaining to controlled substances is found in the Controlled Substance Act; Title 21 United States Code (USC) sections 801-971 (specifically sections 821-829); Department of Justice Drug Enforcement Agency (DEA) Clarification of Registration Requirements for Individual Practitioners 21 Code of Federal Regulations (CFR) Part 1301; and Texas Occupations Code Title 3 Health Professions Subtitle B Physicians (“medical practice acts”) Chapter 157 Authority of Physician to Delegate Certain Medical Acts.
Additionally, registered nurses are governed by the Texas Occupations Code Title 3 Subchapter E Regulation of Nursing (“nurse practice acts”) Chapter 301 Nurses. Section 301.154 section (a) states the following: Rules regarding delegation of certain medical acts. (a) The board may recommend to the Texas State Board of Medical Examiners the adoption of rules relating to the delegation by physicians of medical acts to registered nurses and vocational nurses licensed by the board. In making a recommendation, the board may distinguish between nurses on the basis of special training and education. Further, chapter 222 of the Texas Board of Nursing Rules and Regulations relating to Nurse Education, Licensure, and Practice states that for approval of prescriptive authority, an RN shall “have full licensure from the Board to practice as an advanced practice registered nurse” and submit an application with evidence of successful completion of specific graduate level courses.
Subsection 157.0511 of the medical practice acts indicates the following: Prescription Drug Orders (a) A physician’s authority to delegate the carrying out or signing of a prescription drug order under this subchapter is limited to: (1) dangerous drugs; and (2) controlled substances to the extent provided by Subsection (b). Subsection (b): A physician may delegate the carrying out or signing of a prescription drug order for a controlled substance only if: (1) the prescription is for a controlled substance listed in Schedule III, IV, or V as established by the commissioner of public health under Chapter 481, Health and Safety Code… (4) (b-1) The board shall adopt rules that require a physician who delegates the carrying out or signing of a prescription drug order under this subchapter to register with the board the name and license number of the physician assistant or advanced practice nurse to whom a delegation is made. The board may develop and use an electronic online delegation registration process for registration under this subsection.
(c) This subchapter does not modify the authority granted by law for a licensed registered nurse or physician assistant to administer or provide a medication, including a controlled substance listed in Schedule II as established by the commissioner of public health under Chapter 481, Health and Safety Code, that is authorized by a physician under a physician’s order, standing medical order, standing delegation order, or protocol.
The Texas Department of Public Safety governs the Texas Prescription Program which regulates the dissemination of controlled substances to consumers in Texas. According to the DPS website, http://www.txdps.state.tx.us/RegulatoryServices/prescription_program/prescriptionforms.htm accessed January 12, 2012, “Every Official Prescription form, produced from January 1982 through the present, contains the practitioner’s DPS and DEA registration numbers, a unique control number and the DPS seal (as a watermark) on the face of the prescription. The modifications to the Official Prescription forms do not invalidate previously issued prescription forms. An Official Prescription form is considered valid if it contains the security features associated with that particular format/layout and the practitioner’s DPS Controlled Substance Registration number is current and valid.” Further, the DPS drug rules, subchapter D section 13.81 indicates specific actions to be taken if a prescription for a controlled substance is questionable, to wit: If a dispensing pharmacist receives an official prescription form that creates a substantial question or doubt in the mind of the dispensing pharmacist, the pharmacist must, before filling the prescription, communicate with the prescribing practitioner in order to resolve the question or doubt. Additionally, Section 481.061 Subsection 2 (h), of the Texas Health and Safety Code was amended to include the following rule “ A pharmacist may dispense a controlled substance listed in Schedule III, IV, or V under a written, electronic, oral, or telephonically communicated prescription issued by a practitioner defined by section 481.002 (39) (C) and only if the pharmacist determines that the prescription was issued for a valid medical purpose and in the course of professional practice…“
The available resources repeatedly indicate the requirement of the DEA# and registration in the DPS controlled substance registration program. Registrants in the Texas DPS controlled substance program may use the specified form which has the DEA# and DPS# preprinted on the prescription form. An advanced practice nurse who has satisfied all of the applicable state and federal requirements, may indeed prescribe controlled substances in Texas. However, an advanced practice nurse may also facilitate a prescription for controlled substances as a delegated duty from a supervising physician. In this capacity, the signature on the prescription form of an advance practice nurse acting on behalf of the supervising physician is the same as a valid signature from the prescribing physician. If, hypothetically, an error or omission is noted on a prescription form – the pharmacist has a duty as indicated in the above referenced statute to contact the prescribing provider to clarify the suspected error or omission.
Let’s use an example that may illustrate the importance of being aware of this law: Let’s say a CRNA has a DEA# because they have at one time practiced as a locums provider in an arrangement that required the individual CRNA have their own DEA# (i.e. without a supervising physician or “medical direction”); then the CRNA changes practice arrangements (i.e. relocates or takes another locums assignment) to a facility, which has its own DEA#, and permits advanced practice nurses practicing within the facility, (with or without “medical direction”), use of the facility DEA#……..Hmmm Such a set of facts might prompt a call from the DEA to inquire about your DPS number. Why? DEA #’s are specific not only to the provider to whom they are issued, but they are also specific to one facility or one state.
Keep in mind, our legislated laws are written for the masses. Thus laws that are designed to cast a very wide net, may inadvertently harm some of the small fish. Forewarned is forearmed.
Additional resource:
http://codes.lp.findlaw.com/uscode/21/13/I/C
About the author: Pamela Chambers is a staff CRNA a Central Texas regional trauma center and the affiliated Children’s hospital. Ms Chambers received her MSN in 2000 while on active duty in the U.S. Army; then received her Executive Juris Doctor (EJD) in Health Law in 2008 from Concord Law School. Ms. Chambers owns Lex Terrae Consulting a health law research and consulting firm and also teaches Legal Nurse Consulting for Kaplan University. Ms. Chambers is not an attorney. The information provided is legal research and should not replace consultation with an attorney or physician when warranted. Click here to learn more about Lex Terrae Legal consulting services.
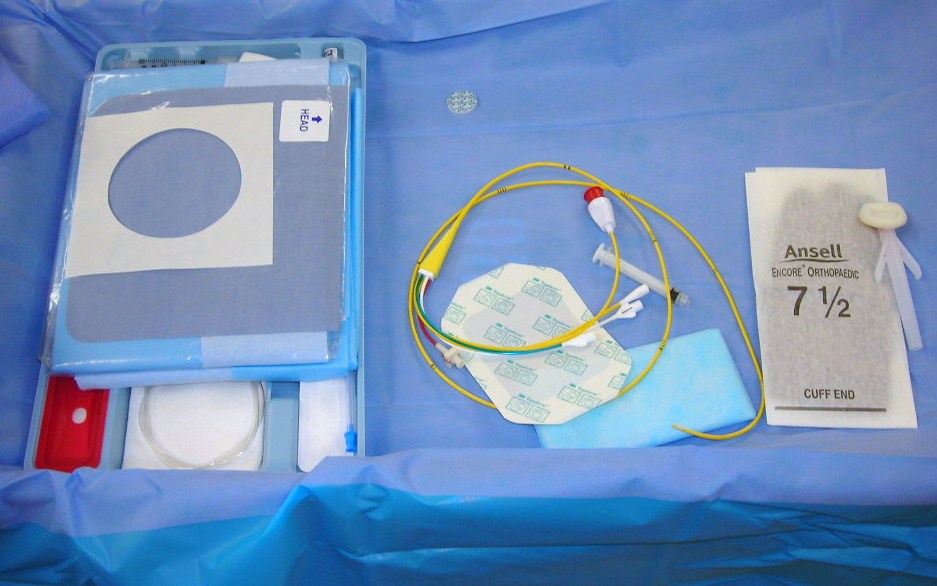
 For nearly 60 years ultrasonography has been in use in clinical medicine. Over the past few decades the use of ultrasonography in anesthesia has increased. As imaging machines improve in technology and the use of ultrasonography becomes everyday practice, patients are benefiting in terms of safety, comfort and cost. The number of hands on workshops to teach anesthesia providers the proper use of ultrasonography is an indication of the importance and popularity of the technique.
For nearly 60 years ultrasonography has been in use in clinical medicine. Over the past few decades the use of ultrasonography in anesthesia has increased. As imaging machines improve in technology and the use of ultrasonography becomes everyday practice, patients are benefiting in terms of safety, comfort and cost. The number of hands on workshops to teach anesthesia providers the proper use of ultrasonography is an indication of the importance and popularity of the technique.